Community-Centered Health
In communities across the state, diverse partnerships of stakeholders are working together to break down barriers to good health.
Background and Approach
Community-Centered Health is our long-term approach to increasing the capacity of North Carolina communities to act on the root causes of health and health disparities by investing in diverse multi-sector partnerships that amplify community voice in setting local health priorities.
Since the initial implementation in 2015, we have supported two cohorts of grantees. Each work across sectors, and with community members, to identify their most pressing issues and develop collaborative strategies that focus on system and policy changes to influence health. Within each community, partnerships have received multi-year grant funding along with non-monetary technical assistance, training, coaching, and convening support.
Our first cohort of Community-Centered Health grantees included collaborations in Asheville, Gastonia, and Greensboro. Supported by more than $2 million in investments, these communities realized positive results in local policy, environment, and systems changes. Direct grant support for these three communities concluded in 2023.
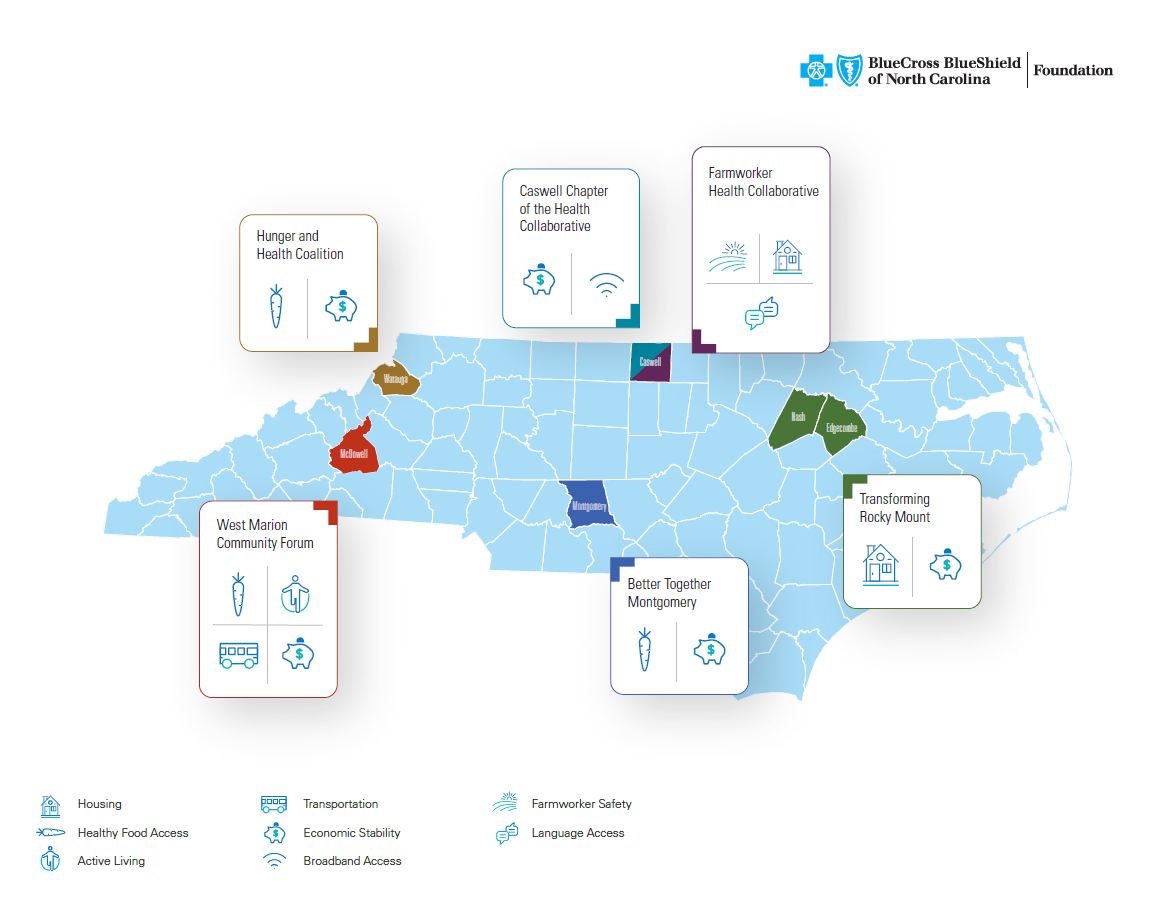
In 2019, we added six additional communities, forming the second cohort of Community-Centered Health grantees. These communities were supported with an initial 15-month planning grant and are now part of a $7.5 million commitment to further support and learn from their work.
Current Cohort Community Profiles
BETTER TOGETHER MONTGOMERY
Location: Troy
Areas of Focus: Healthy Food Access, Economic Stability, Access to Care, Physical Activity
Montgomery County is located in the south-central region of the state with a population of less than 30,000. As a result of compounding economic and social factors, county residents face barriers to healthy food purchases, which have contributed to many health complications. Better Together Montgomery is working to reduce the prevalence of obesity, heart disease, high blood pressure, arthritis, and diabetes while increasing food security and economic stability specifically in rural, African‐American communities around Troy and Candor. They are also working to improve residents experience with the local health care system which led to the creation of a Patient Advisory Committee in 2020.
More About Better Together Montgomery:
CASWELL CHAPTER OF THE HEALTH COLLABORATIVE
Location: Yanceyville
Areas of Focus: Economic Stability, Broadband Access, Community Wealth Building
Caswell County – located on the North Carolina/Virginia border – is home to 23,000 residents, many of whom were born and raised in the community. Today, economic instability, food insecurity, chronic disease, and poverty rates are prevalent within the county. The Caswell Chapter of the Health Collaborative has focused on building a collaborative, inclusive partnership addressing inequitable access to resources through community wealth building. In addition, the partnership is working to create physical and social infrastructures to foster greater social cohesion, increase access to broadband, enhance local economic development opportunities, and strengthen its local food system to integrate sustainable food production, processing, and distribution.
More About the Caswell Chapter of the Health Collaborative:
FARMWORKER HEALTH COLLABORATIVE
Location: Caswell County
Areas of Focus: Occupational Health, Chronic Illness, and Employment.
In North Carolina, there are an estimated 118,000 farmworkers who are largely uninsured, earn wages that place them below the Federal Poverty Line, and many of whom live in employer-provided housing in rural areas, isolating them from health care services. The Farmworker Health Collaborative serves rural areas of Caswell County and seeks to elevate small community-led projects focused on farmworker and poultry processing worker populations related to occupational health and chronic illness by focusing on access and employment in Caswell County.
More About Farmworker Health Collaborative:
HUNGER AND HEALTH COALITION
Location: Boone
Areas of Focus: Healthy Food Access, Economic Stability, Housing
Hunger and Health Coalition is situated in Watauga County, which has a population of less than 60,000, more than half of whom live in rural areas. Watauga County also has the third highest poverty rate in the state, with residents facing lack of affordable housing and food-insecurity among other challenges. Hunger and Health Coalition is expanding and strengthening efforts to reduce obesity and diet‐related chronic diseases in low‐wealth populations with a focus on food insecurity through its Food is Medicine program. This includes expanding screening for food security in physician offices, connecting patients with medically tailored food boxes and nutrition education, and building community leadership across the county to support healthy eating.
More About Hunger and Health Coalition.
TRANSFORMING ROCKY MOUNT
Location: Rocky Mount
Area of Focus: Housing
Rocky Mount is located in northeast North Carolina where it straddles Nash and Edgecombe counties. Transforming Rocky Mount is working in marginalized communities to support residents in implementing systems‐focused solutions to reduce stressors in their physical and social environments that have contributed to a high prevalence of chronic disease and depression. They have laid the groundwork for more direct community input into local government decisions and have made notable progress toward city policy on housing and development. This work is focused in low‐income, African‐American communities in Edgecombe and Nash counties that are impacted by a long history of housing segregation.
More About Transforming Rocky Mount.
WEST MARION COMMUNITY FORUM
Location: Marion
Areas of Focus: Healthy Food Access, Active Living, Transportation, Economic Stability
West Marion Community Forum is based in McDowell County, nestled in the foothills of the Appalachian Mountains with more than 70% of the population designated as rural. While positive revitalization efforts and new partnerships have ignited change, historic disinvestment and a decline in the manufacturing industry, among other factors, have resulted in poverty, substance abuse, and high rates of chronic disease. West Marion Community Forum is working with historically excluded residents in African‐American and Latino communities to address food insecurity and obesity in children ages 0-5 and their caregivers. West Marion Community Forum has created a successful toolkit outlining their approach and have received positive attention and interest from other communities looking to replicate efforts. Their collaborative has a mantra – shift happens for the health of our community – that defines their work.
More About West Marion Community Forum:
Initial Cohort Community Profiles
COLLABORATIVE COTTAGE GROVE
Location: Greensboro
Areas of Focus: Healthy Affordable Housing, Healthy Food Access, Active Living
The Cottage Grove neighborhood in Greensboro is extremely diverse, with many languages and a variety of cultures represented. Years of disinvestment resulted in challenging and inequitable conditions for these neighbors. Using the Community-Centered Health approach, Collaborative Cottage Grove worked to improve housing and neighborhood conditions to reduce the severity of asthma and other respiratory conditions and increase access to healthy food. Neighbors actively led work to advocate for healthier, affordable, housing conditions by engaging with local universities, community health workers, and city leaders to improve neighborhood infrastructure and food access.
More About Collaborative Cottage Grove:
HEALTHIER HIGHLAND
Location: Gastonia
Areas of Focus: Active Living, Infrastructure, Health Care Access
Healthier Highland is centered in a historically African-American community in Gaston County, not far from Charlotte. Years of disinvestment and other factors resulted in unhealthy conditions for those who call the neighborhood home. Using the Community-Centered Health approach, Healthier Highland built a culture of healthy eating and active living in the Highland community by engaging resident-leaders, building a neighborhood association, and strengthening partnerships between local organizations and the hospital which, through the BUILD Health Challenge, has made a significant investment in community health.
More About Healthier Highland:
MOTHERING ASHEVILLE
Location: Asheville
Area of Focus: Healthy Birth Outcomes for Black Babies and their Mothers
In western North Carolina’s Buncombe County, African-American babies die at three times the rate of their white counterparts. Many factors, among them limited health care access and structural and institutional inequities have contributed to this alarming disparity. Using the Community-Centered Health approach, Mothering Asheville works to reduce, and ultimately eliminate, racial disparities in infant mortality by changing institutional policies. In partnership with a safety net obstetrical practice, this collaborative has developed a doula program that employs women from the community most impacted by infant mortality to provide lay services to pregnant women from their own community.